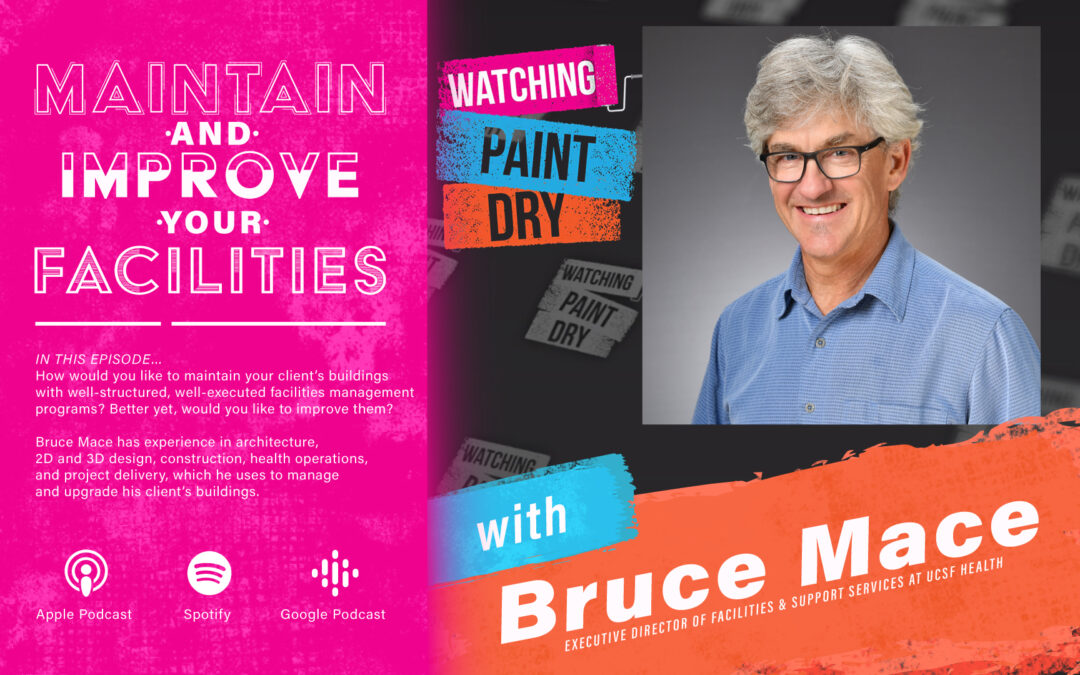
Bruce Mace is the Executive Director of Facilities and Support Services at UCSF Health, one of the nation’s top 10 hospitals. Bruce has extensive experience in architecture, 2D and 3D design, construction, and project delivery. Over the past 15 years, Bruce turned to healthcare operations and has developed dedicated teams of professionals in the areas of safety, energy, leasehold, construction, call center, operations, and business applications.
Here’s a glimpse of what you’ll learn:
- Bruce Mace talks about UCSF Health and the new building they are constructing
- What challenges did they face while expanding UCSF Health during the pandemic?
- Bruce explains how they’ve maintained their structures during the pandemic to meet hospital accreditation standards
- The lessons Bruce and the UCSF Health team learned from the pandemic
- Bruce explains the importance of having a backup plan in the event of an emergency
- New technology and tools in the construction industry
- Bruce shares his background and how he transitioned to facilities management
- How can you make data entry more efficient with a new building?
- Bruce’s advice for people wanting to work at UCSF Health
In this episode…
How would you like to maintain your client’s buildings with well-structured, well-executed facilities management programs? Better yet, would you like to improve them?
Bruce Mace has experience in architecture, 2D and 3D design, construction, health operations, and project delivery, which he uses to manage and upgrade his client’s buildings. Today, he shares lessons he has learned over the past 15 years to help others refine their facilities and boost their business.
In this episode of Watching Paint Dry, Greg Owens sits down with Bruce Mace, the Executive Director of Facilities and Support Services at UCSF Health, to discuss ways brands can maintain and improve their facilities. Bruce talks about the challenges they’ve faced expanding UCSF Health during the pandemic, the lessons they’ve learned and the importance of having a backup plan, and new technology and tools in the construction industry.
Resources mentioned in this episode:
- Greg Owens on LinkedIn
- McCarthy Painting
- McCarthy Painting Contact No.: 415-383-2640
- McCarthy Painting Email Address: info@mccarthypainting.com
- Bruce Mace on LinkedIn
- UCSF Health
Sponsor for this episode…
This episode is brought to you by McCarthy Painting, where we serve commercial and residential clients all around the San Francisco Bay area.
We’ve been in business since 1969 and served companies such as Google, Autodesk, Abercrombie & Fitch, FICO, First Bank, SPIN, and many more.
If you have commercial facilities in the San Francisco Bay Area and need dependable painters, visit us on the web at www.mccarthypainting.com or email info@mccarthypainting.com, and you can check out our line of services and schedule a free estimate by clicking here.
EPISODE TRANSCRIPT
Intro 0:10
Welcome to the Watching Paint Dry Podcast where we feature today’s top leaders, industry experts and more to discuss issues affecting facility managers and property owners. Now let’s get started with the show.
Greg Owens 0:23
Hello, everyone, this is Greg Owens with Watching Paint Dry Podcast where we are continuing our discussions with facilities, managers, property owners, business owners, the entire support system out there that keeps buildings going and keeps the environment clean inside those buildings and keeps it safe for the people that are using those buildings. This podcast like all our podcast is sponsored by my company McCarthy Painting, you can find out more about McCarthy Painting, go to McCarthypainting.com. We do both interior and next year are super glad to be on a bunch of interior work right now. Because it’s raining in San Francisco, which we really need it as much as it messes up our exteriors season. It’s great to see the rain, it feels wonderful to have it and hopefully keeps us from having that horrible fire season that lasts so long like it has been in the last few years. We’ve done all kinds of projects. We’ve been doing a bunch of work for some of the autonomous vehicle companies, which is super interesting to see what they’re up to. I love getting inside new startup companies and seeing the actually like the cars that they’re making to be autonomous taxi cars and that kind of stuff. And we’re painting for some of those companies right now. And it’s been fun. today. I’m really excited to have Bruce Mace on this podcast. Bruce is the executive director of facilities and support services for UCSF Health here in the San Francisco area. Welcome, Bruce.
Bruce Mace 2:04
Good morning. And thank you Greg.
Greg Owens 2:05
Yeah, and so and tell me like UCSF we just talked about a little bit. You’re involved in the hospital side of things, not necessarily the research side of things.
Bruce Mace 2:18
That’s accurate. UCSF was a big organization. And we’re broken up into parts and I’m on the academic medical side. So health or hospitals.
Greg Owens 2:30
Right? And what are the other parts because I don’t really know much of I mean, I’ve gone to the UCSF I’ve been to Parnassus location, your Parnassus location. And I’ve been to the Mission Bay location. I think I went there for a knee problem that I had. And it didn’t go away. The lady told me like, this is your picture of your cartilage. And this is where the cartilage is missing. And I was like, well, what can we do about that? Is that nothing right now is like 10 years ago, but my knees are doing really well. Lately knock on wood. Maybe just finding out help.
Bruce Mace 3:13
I can’t take credit for that.
Greg Owens 3:17
Well, sometimes knowing that you can’t do anything is helpful. I find it helpful, right like okay, you know, we just move on live life and move on. Right. And what was the other location for the hospital.
Bruce Mace 3:30
We have hospitals at Mission Bay Benioff, Children’s Hospital in Oakland, Mount Zion hospital and Parnassus, Moffett long or big hospital on the hill and Langley Porter psychiatric institute, which we are currently in the process of moving the clinical aspect over to the Mount Zion location.
Greg Owens 3:53
Oh, wow. Yeah. So then you’re going to keep that location.
Bruce Mace 3:58
Well, Mount Zion stays and LPI where it’s currently located on park at Parnassus. It will be torn down in the next 24 months to make way for what’s currently called new hospital at Parnassus heights, which is a 15 to 18 Storey, new tower, providing a lot more capability at the Parnassus site.
Greg Owens 4:20
Right, right. Boy, that must have taken some time to get that approved through in the city of San Francisco. That’s got to be hard.
Bruce Mace 4:27
Years worth. Yes. We’re still in the process of approvals.
Greg Owens 4:34
Wow. It’s I mean, people don’t like change, right? Especially if it’s changed. They don’t get to be involved in and it’s always amazing to me how much resistance we can get. Because like the dealing with old buildings is incredibly challenging and people don’t realize that right? And so sometimes it’s better rather than like trying to remodel this old building. It’s so much better and useful. Just tear the whole thing down and start over. because you can build it from the ground up with the new technology that we know about today to make it a more functional building. Right.
Bruce Mace 5:07
Yeah. And in this case, you’re touching on something that this new hospital tower is coming up alongside of and connected to existing Moffitt long hospital. So it’s actually a marriage of the old and new with a 70-year disparity in between. It’s a whole another flavor to the equation.
Greg Owens 5:30
Yeah, it’s such a hard debate to have, because, because there’s some, there’s this the historical significance of that building is why they’re keeping it right.
Bruce Mace 5:41
Part. Yeah, the historical part of it. And then also, the value what systems are worth keeping, and placing versus tearing down a smaller building, augmenting, and bringing the whole MOSFET long hill to a newer sort of position?
Greg Owens 6:01
Yeah, yeah. There’s so many things to consider. But it does escalate the cost when you try to merge those two types of buildings and facilities so that they can work seamlessly together. And then the and then, and then the architectural side of it. I mean, they’ve been doing some great things with blending the two, right, and making it really work well, these days, much more so than I think when I was a kid in the 80s, or 70s.
Bruce Mace 6:31
Yeah, there’s obviously, the group, the Design Group, which is worldwide and world-class, working together to come up with a design that incorporates the old and new and sort of blends the demarcation line on a visual sort of stance, and then what happens behind the walls above the ceiling, with systems and new systems, old systems and things that certainly weren’t even around, 40, 50 years ago, how do we do that kind of work?
Greg Owens 7:04
Right, like basic things that we take for granted in new construction, like air conditioning, or proper ventilation? It’s almost non-existent in buildings 30 or 40 years ago, comparatively, I mean, it’s there, but not the same level or same technology at all.
Bruce Mace 7:25
Yeah. And especially coming hopefully be in sort of at a low or a tail end of our pandemic, in a changing season. What did what happened two years ago with the arrival of COVID mean, for old buildings with limited capabilities, versus, say, our new Mission Bay Hospital down there on the flats, where we had a lot more control and capability two different approaches.
Greg Owens 7:53
Yeah, tell me about the challenges. What made it easier over there at the Mission Bay location, which is, you said, five years, it’s been built five years ago, brand new building, brand new, I mean, everything there is super easy and parking’s easier, and all of those things. So I think that’s probably part of it. What else played into that during this pandemic?
Bruce Mace 8:16
Well, certainly with the arrival of COVID, and the initial months and days and hours of realizing that we were, you know, not watching something from the other side of the world, but that it was on its way, and it was going to be here. And then as it arrived, East Coast moving west, we had a little bit more time than most. But the realization that transmissibility, how do you transmis a disease like that, and the vet air was going to be probably, at that time, the most important component. So what do we do with our air, with pressurization with air exchange filtration, how do we use those tools in a new building versus an old and certainly at Mission Bay, where we have control systems that allow a lot more monitoring, visualization of current state, and then also the control to change settings to move air or filter, air exchangers, such that it benefits the fight against, you know, something like COVID?
Greg Owens 9:22
Right. Because you can customize it to the room to the location to the building, you probably can even separate it was probably easier to separate or compartmentalize if you needed to. Yeah, and an old legacy system, you don’t have that ability to press a button and sort of like cut off one part from another part or change up the volume of air that’s moving through it.
Bruce Mace 9:48
That’s absolutely correct. So down at the Mission Bay, it was more of a controls effort, and it was working from systems that are in place and allowing us the ability to change and manipulate modify those settings versus up at Parnassus where our high acuity patients are starting to roll in at the beginning of COVID. And you’ve got already very technical spaces in the intensive care units that are now we’re modifying, but it’s a physical modification to rooms done by real people, as we’re bringing in COVID patients. So the idea of working actively in those environments as well was a big deal.
Greg Owens 10:30
I can only imagine that Parnassus because Parnassus is an old, how long ago is that building built between two series of buildings?
Bruce Mace 10:39
Yeah, the major build period for between the two is 55 to 75 years ago, so it’s been a while.
Greg Owens 10:47
The last time I worked that on Parnassus, because I’ve been there but I’ve also worked on it. I painted the flagpole on Parnassus, my saw, climbed it, my uncle had a company. McCarthy painting was started by my Uncle Fred McCarthy and Fred was a steeple Jack and he learned it from his father in New York, and they painted flagpoles. I quit high school at 16 and started working with my uncle. And we specialized in painting flagpoles at that time, right in the San Francisco Bay area. So I climb most of the wooden flag poles throughout the San Francisco and some of the steel ones too. And we went over there and painted that one to a long time ago when I was probably 18 years old. And we’re talking like 30 years ago. It’s a young it’s a young person sport to climb the climb flagpoles, right? So you’re doing it physically?
Bruce Mace 11:41
Oh, yeah. I’m sure, that’s got to have its risk and reward as well.
Greg Owens 11:47
Yeah, it was a lot of fun to do. Because you climb it, you go up prepping, you come down priming, you go back up, and then you come down and painting and you go back up, and then you come down painting. You don’t want to paint yourself into a corner on a flagpole. But that building I can only imagine all of the challenges. It’s a challenging building, regardless, like I go there, and I have an appointment with a doctor and defined the office and the building and the place and go through the elevator system. And it’s one building connecting to another, and they’re not the same at all. And each, it’s very confusing, right? I can only imagine during the pandemic, that like just escalated, because it’s also tight spaces. It wasn’t built with big, wide open lobbies, and things like that, and not tight sort of narrow corridors, right. And what there wasn’t a lot of the same thought process that might be done into a hospital these days.
Bruce Mace 12:45
Yeah, you’re correct there. And then, and specifically, infrastructure, you know, 60 to 75 80 years ago was very, very different. And the systems that served the hospital were a lot more simple. They weren’t as complex, they didn’t take up as much space. And so the interstitial space between a ceiling and a seven year old hospital and the upper deck is a lot different than say what we’re building into new hospital, such that a 15 storey building 60 years ago is now equates to about 19 stories, when you figure in all the extra interstitial.
Greg Owens 13:21
Oh, interesting, because they want to make sure there’s a space for all the mechanicals between each floor so that you can add new things, or new things or big things and do the maintenance. These are things that they consider now, which they didn’t really have or consider back then.
Bruce Mace 13:38
Absolutely. Yeah. And also the tools that are used to design new hospitals, the architecture, the models, the 3d, and how do we use those tools to move forward and solve some of the problems that we’ve had in the past?
Greg Owens 13:54
Right, right. And we ain’t know. And then 67 years ago, they didn’t have the same level and amount of people too.
Bruce Mace 14:01
Yeah, the volume of people and activities and the clinical processes have gotten more complex and denser and higher acuity are certainly doing things that weren’t done that many years ago?
Greg Owens 14:13
And did you guys have to change up? I mean, I’m assuming you must have had to change up completely how you did things during the start of the pandemic. And then during the pandemic, did you have to, like move things over to the Mission Bay that were more critical there like, how did you guys look at all your structures together during this pandemic?
Bruce Mace 14:37
Yeah. From a clinical perspective, Parnassus, Moffitt long as our super high acuity adult hospital, and so all the systems that are there to support that kind of patient population, they’re built in, they’re there and they’re not moving anywhere else. And so it immediately became sort of, okay, how do we modify environments to better suit, the work that needs to be done. And early on, after a few months in we’re modifying environments and air flows. And early on CDPH and H Kai are our building official. In essence, for hospitals here in California, they issued sort of a, not even sort of it was it was a waiver, which gave us a lot more leeway to do what we need to do with environments without having to go through extended sort of plan, review and such. So we’re coming out of that operational period here and another two months, but it was unheard of it just simply has not happened in modern times.
Greg Owens 15:41
Because hospitals have special regulatory oversight. Not including like food and beverage, right, like, we don’t even go there. That’s craziness in its own right. But just for the basic, like health care facilities have a different set of guidelines and an oversight by the city by the state and by probably it was also federal, but basically, I would think that the city and the state gave you more leeway to make changes, as you saw needed for your work staff, your buildings to sort of help deal with.
Bruce Mace 16:17
Yeah, and I would sort of like it. I’ve explained to others that UCSF health is sort of a large ship at sea, where we’re given fair autonomy from city regulation. And we react to HSI, the state organization, official for the state of California. And they’re closely tied with California Department of Public Health. So our general rules come out of those regulatory entities, and in something called hospital accreditation standards, and those are, it’s straight from code, from our code that everybody would recognize, but carefully selected spectrum of preventative maintenance and infrastructure protections and such that we have to perform and document on a daily basis.
Greg Owens 17:09
Yeah, I’m remembering. I’ve done a bunch of work for health care facilities, and some of the aspects of the health care facilities fell underneath that. And I remember back when we were doing some construction work, and some of them, we had to deal with some of those other agencies.
Bruce Mace 17:23
That’s it seems.
Greg Owens 17:27
Oh, man. And so during this pandemic, I’d love to get a little bit of your perspective, because I stopped watching the news, because I couldn’t one, there was so much I couldn’t do about it, I realized, right, and this has happened to me a few times in my life where it was better for me to focus on what I could actually control, than keep hearing about things that I had no control over. And that one of those was like the hospitals getting overwhelmed. And I would hear certain things, but it was hard to like, really sort of find out what was happening. From your perspective, were you guys like, overwhelmed at times during this? Or from your perspective, was things like, kind of controlled chaos in a way? I mean, it’s still chaos, because we don’t know all the things. How did it feel for you going through it?
Bruce Mace 18:17
Yeah, that’s a good question. And it is also multi-tiered, I think in the risk response. Early on, we’ve at a leadership level, in our meeting, daily discussing COVID. And what it meant, when it was still across in Europe, and in the Middle East, as we saw it coming in started to prepare, we were meeting on site, all of us are there and sitting in a room, and we’re discussing what we’re going to do. And I can remember the day, we’re all sudden, it’s here, and people were looking around, and it was like, this is the end of it. We can’t meet in here anymore. It’s real. It’s here. And we were well underway with our, trying to build in precautions and capabilities. So there was the reality of it moving from a TV screen, something that’s happening elsewhere, to went through New York and cause devastation.
Greg Owens 19:13
Severe devastation in the retirement homes and some hospitals, for sure.
Bruce Mace 19:19
And in hospitals. And so we’re talking with colleagues and compatriots back there on a daily basis, we were sending teams to support and it was sort of a, it’s coming, it’s here, and then I don’t want to get too political. But I think decisions that were made by our governor and our mayor here in the Bay Area may add significant impact on what we felt later on being less than maybe some other areas. So there was that aspect to it. And then it was, how do we change our environment the feeling of, you mentioned being able to walk away from it or sort of turn ahead and focus on what do you do? What do you do best? Well, we have a job. And my team is just unfathomably good and dedicated and everybody there every day, and really putting heads together doing white paper research and talking to colleagues across the globe and trying to figure out, what is the best that we can do, given the knowledge that we have today? And that certainly changed over time. Yeah, but it was that inability to get away from it. Almost that was the scariest.
Greg Owens 20:33
Yeah, because you still, even though I think certain aspects of the hospital definitely closed down, or they stopped doing certain types of surgery that was needed right away, but there was an entire different other departments that were being overwhelmed. And you guys still have to come in and do your role, your team still has to come in every day and problem solve and figure out and not new things that are coming in, but also like the legacy things that you always have to take care of Anyway,
Bruce Mace 21:05
yes, yeah, you have to keep up with all of your preventative maintenance, all of your work that takes place, at the same time modifying environments, keeping track of modifications, and what we’re doing and why and being prepared to discuss why with whomever should come and ask for that sort of documentation. And then, the fact that people are in the field, right, and at the time, what you can’t see can hurt you. And what do we know, and it was a it’s a daily sort of information dissemination to crews and teams about an ever-changing PPE requirement, and how do we best protect. So it was a real fine dance and then watching our clinical partners, where the ICU is going crazy, they’re exploding in volume. And like you say, at the same time, the enterprise making decisions about how we can tune down, if you will, you know, elective surgeries such that we can reallocate resource to where we’re being hit the hardest. So it’s an interesting time to watch a large hospital in motion really proud of it.
Greg Owens 22:15
But yeah, a large hospital in a major city. Right. This is not small town. Yeah, so you are definitely the Ground Zero playing triage on a daily basis with your role, I would think, right, because certain things, you definitely have to shelf and say like, that’s not important right now, we’ll have to come back to that in six months. Because the six months shelf is the two months of here’s the immediate, like, we need to be on these things.
Bruce Mace 22:47
Now. You’re absolutely right, watching the intake down through our IDI and what was happening with our emergency department, all of our clinical partners there, and just the incredible pressures they were facing, and a real time feeling of how can we help? What can we do to that environment, to modify it to provide protections to those clinical groups? So it became exercise and in teamwork, and how good of the organization how they perform?
Greg Owens 23:21
Yeah. And then, like you said, like, numbers-wise, definitely, what the city of San Francisco seemingly did a better job or knowing better, maybe that’s not quite the right word, but managed it differently. And what we know the numbers have been better than some other cities of a similar size, right? And I’m really curious about like, 10 years from now, when the studies really come out. So it takes time you accumulate all the data, like what worked and what didn’t work and see what because people were sort of making things up as we go. Like you said, early on, everybody was like, my girlfriend was like washing everything that came into the house. Like scrubbing things down with gloves, and PPE and all that, right? Not many people are doing that anymore to that level. Right?
Bruce Mace 24:10
That’s correct. And it changes flavor and upfront where they weren’t positive about the way it transmits.
Greg Owens 24:19
Right, it was a mystery for a long time. They were accumulating data, right, like for a long time, and then they’ve slowly backed away from some of the things that I don’t even know if some of them were recommended. It’s just that people started doing it.
Bruce Mace 24:33
Yeah, exactly. And as an institution, we certainly have learned an incredible amount. And then like you say, the white paper and the look backs and the studies that are all rolling out and have been rolling out are beneficial to the future. And we’re in a interesting position where we’re in design for this new hospital. So at the same time, where are trying to roll out at COVID, we have all this new experience that we’re trying to roll into the new hospital.
Greg Owens 25:06
Are you making those changes to the new hospital as we like you? Yeah. So you really looked at it and said, hey, the way we thought of this two years ago, is different. We need to really rethink about the world that we know now, based on some new data. Wow. Anything that you can talk about that you specifically in that?
Bruce Mace 25:27
In general, I controllability and the ability to break floors and units and rooms into smaller subsets that have air that performs or is controlled to perform independent of other areas. Breaking down shared plenum space, or shared duct space for exhaust and supply, you know, giving ourselves building in the ability to with controls, change environments, and then flex up and flex down, because that’s been the thing that I don’t think a lot of people see from the outside is this thing has been in waves, right? So it’s flexing up flexing down. And what can we do to make that work process or pattern easier for all concerned? Is a big one going into the new hospital. And then how do we filter? How do we add capability to filter to higher standard or even with the fires the wildfires to smell and particulate that we don’t want in a hospital. So, yeah, a lot of really interesting working sessions that go on going into the new hospital.
Greg Owens 26:42
Yeah, I learned a lot about Air and Air Quality from the podcast I had with the facilities manager. I can’t remember his name right now. But he’s the facilities manager for the San Jose School District. High schools, right. But they have like, 19,000 kids going through a building a day. Did you listen to that podcast?
Bruce Mace 27:03
I did.
Greg Owens 27:06
His not knowledge of this subject precedes the pandemic, right? He was working on it before because of co2 levels. He had a high concern for co2 levels, because he noticed like teachers were having headaches and problems and different things like that. And he started to figure out like, Oh, if compartmentalize and really make it so that the air quality looking at the air quality based on the use, by the minute that they can save a lot of money, energy and get the money that way. Right. And it was turns out that they were able to save a lot of energy, but then it turns out that it was perfect knowledge for COVID and pandemics.
Bruce Mace 27:46
Yeah. So it’s our environment. And what we can’t see is incredibly critical, you know, if it’s high school kids falling asleep, because they don’t have enough oxygen that they’re at their desk, and teachers with headaches. Or if you’re in an ICU, and you’ve got something that you don’t want other people to have. So air has to stay inside of a room and be exhausted out versus there are those that it’s got to be a positive environment because they’re so immunocompromised and vulnerable, there’s a vast spectrum in between.
Greg Owens 28:18
And they think you guys will be cutting edge around that going into the future of how to customize per room, basically, in so many ways or per floor per unit or what the use is, but I also see that I think going forward for almost all construction is going to start looking at it that way.
Bruce Mace 28:38
I think we’re gonna see profound changes in design and construction in our built and living spaces in the coming years. As much as Northridge earthquake did for structural COVID has done for environmental.
Greg Owens 28:52
Environmental. Yeah, which is good, I think as bad as this pandemic is, it could be really good for cutting edge new sort of technologies to really put that focus on the health of a building and that environment. Right. And like you said, we also have the added challenges of fires and things like that being able to filter our air rather than just bringing it straight into the building because there’s been Cooperman, like during the pandemic there was it was a few days that San Francisco, I live in Marin and I could see San Francisco and it was a few days you couldn’t see San Francisco because of all this smoke, right. Like you can see the sun.
Bruce Mace 29:33
Yeah, exactly. And I mean, depending on what we see with global warming, or you sit there, we’re seeing tip of the iceberg, right. So what sort of challenges are we going to have and where we’re a COVID requirement might be directly in competition with a smoke component from wildfires, right and at the same time, you’re under duress from electrical supply, distribution system that passes through national forests and may be burning.
Greg Owens 30:05
New challenges. And you guys have backup generators, too, because you can’t even just rely on solar at all, or even backup batteries. And that kind of stuffs, almost all your facilities must have backup generators? I would think.